"Heartbreaking and Dangerous"
Legislators, Citizens Push Back on OB Unit and Other Closures in Rural Maine
The Bar Harbor Story is generously sponsored by Acadia Shops.
AUGUSTA—Multiple Hancock County legislators have cosponsored LD 1578, an “Act to Require the Department of Health and Human Services to Review Disruption to or Removal of Health Services,” which went before a state legislative committee, Wednesday afternoon, May 7.
If passed, the bill, led by Rep Jan Dodge (D-Belfast), would make it so it isn’t quite so easy for healthcare providers to remove services. The bill would create a state mechanism that would allow Maine to respond to healthcare access disruptions. It would also likely make sure that the public is informed about any hospital services that are proposed to be removed.
TESTIMONY AND REACTION
Much of the testimony before the Health Coverage, Insurance and Financial Services Committee focused on multiple Maine hospitals closing their OB-Maternity units.
Mount Desert Island Hospital announced that it would be closing its maternity unit July 1, meaning that babies would no longer be delivered at the hospital. The decision was often referenced during the testimony.
When presenting the bill to the committee, Rep. Dodge said that “residents in my area and many people throughout the state of Maine believe the closure and impending closure” is creating a health emergency in the state.
Citizens believe hospitals eliminating birthing units isn’t in their best interest, she said.
Houlton moms now drive one hour north or two hours south after the closure of their hospital’s OB.
“MDI parents-to-be are hoping to maintain their on-island services,” Rep. Dodge said. Rural midwives and doulas are concerned that emergency hospital services are no longer close by “if something goes sideways.”
“How many young families will not settle in communities that have reduced birthing?” she asked.
Opponents of the legislation stress that a state review of closures can’t change the factors that cause the departments or services to stop.
Jeffrey Austin, the Maine Hospital Association’s vice president of government affairs and communications said Thursday morning that the MHA definitely does not support the legislation.
"We oppose LD 1578. It’s unrealistic to turn over decision making to the state on these tough issues. And these are tough decisions made by hospital leaders in conjunction with their local boards of directors. No one enjoys this. But there is nothing in the legislation that changes demographics, quality, finance or workforce. We oppose,” Austin said.
For doula Sarah Tewhey of Seal Cove, rural hospitals discontinuing maternity services is both personal and complex with large scale implications.
“On March 27, Mount Desert Island Hospital—a place where I have attended dozens of births over the last decade—announced the closure of its OB unit on July 1,” she testified. “The many pregnant women planning to have their babies there this summer and fall were left feeling upended by this decision. The MDI Hospital closure in July will mark the fourth OB closure in 2025 alone, leaving Maine with only 17 birthing hospitals. Nine of those 17 are rural, low volume, Level 1 hospitals and I am afraid for the future of every single one of them.”
Tewhey wrote that it is becoming fundamentally unsafe for pregnant women and babies in the state.
“Hospitals often cite safety risks due to decreasing birth volume as a reason for closure. However, the safety implications of having no local OB access and the very real pressure that closures put on emergency departments and local EMS are an equally important parts of this conversation,” Tewhey explained. “Lack of local obstetric care presents a major safety concern. This is particularly true in a community like MDI with 2-4 million annual visitors, some of whom will inevitably and unexpectedly go into labor or have an obstetric complication while visiting MDI. Those women needing immediate OB care will now be seen in the hospital’s emergency room without access to obstetric providers and/or they will rely on ambulances or LifeFlight to be transferred to a facility that can provide care. This is a bad outcome waiting to happen.”
The lone oral testimony against the bill stated that it is unsafe to have people deliver babies unless they deliver 200 or more babies a year. MDI Hospital also states on its facts page that its OB closure is “due to a significant decline in births and the challenge of maintaining specialized staff for such low-volume care.” There were babies born at the hospital last year.
“We need to ask the question: is it safer to have a trained obstetric team who are attending fewer births per year or to have no local obstetric team at all? This is an incredibly complex problem that involves declining birth rates, outdated MaineCare reimbursement rates, staffing shortages and the expense of keeping small rural OB units open. Ultimately our for-profit healthcare system is just simply non-congruent with supporting something that happens to every single person, which is birth. Rural OB closure has been happening slowly and painfully in Maine for over a decade and in 2025 appears to be accelerating at an alarming rate,” Tewhey testified.
Though the bill pertains to maternity closures, it’s not only about maternity closures and would potentially apply to other services. Worries about the bill included how the hospitals would ensure safe coverage occurs during the review process, particularly if the hospital cannot find medical providers.
State Senator Nicole Grohoski (D-Ellsworth), lead co-sponsor of the bill, said, “In the wake of MDI Hospital shutting its doors … this bill is especially necessary and timely.”
These closures negatively affect maternal health and women’s health those supporting the bill said. Grohoski stressed that decisions like this cannot be evaluated without taking into account the broader struggle of women’s health and rural healthcare, but also it impacts families and influences who lives in a community. When a hospital stops a service, especially without any community input, “they determine who can stay in the community and who can leave. They determine the future.”
Grohoski said the state needs to improve its policy and make it binding. She stressed that the people of Maine are living through a moment, a discouraging and painful one.
State Representative Gary Friedmann (D-Bar Harbor) agreed and gave his support to the bill.
On many levels the state is facing a healthcare crisis, he said, adding that Mount Desert island was recently shaken by two abrupt announcements. The first was when Northern Light closed the Southwest Harbor medical center that served 1,600 patients. The second was when “decision makers” at MDI Hospital announced that they’d be closing the maternity unit.
“It’s unfortunate that our state’s healthcare system has become so fragile that this bill has become necessary,” Friedmann said.
State Representative Holly Eaton (D-Deer Island) stressed MDI Hospital’s importance to pregnant women on unbridged islands and the transportation barriers they face.
“People in my district cannot simply drive a few extra miles to access care,” she said. “It’s not just inconvenient; it’s dangerous.”
Rep. Eaton also stressed that there was no opportunity to discuss the closure in advance and expressed frustration that at a community meeting held to talk about the closure, MDI Hospital officials didn’t answer questions from the community. The situation, she said, “it is heartbreaking and it raises bigger concerns. If one essential service can disappear …”
Then, what else can happen? It was a question that was in the subtext of multiple testimonies, written and oral.
Emily Wright, a registered nurse at Mount Desert Island Hospital, also testified at the Augusta hearing.
“Our town has recently been rocked by the devastating news,” she said. “This is not a sustainable model of health care.”
If passed, she said, the bill would bring transparency and accountability into the process of other closures.
“This bill represents a chance to bring structure, oversight, and collaboration to decisions that have lasting consequences for birthing individuals, babies, and entire communities,” said Ellen DaCorte of Somesville.
DaCorte is the clinical lead RN in the MDI Hospital’s obstetrical department.
“LD 1578 presents a valuable opportunity to formalize the process by ensuring that external experts and key stakeholders are included in a collaborative task force when any health service is at risk. This proactive approach would bring the right voices to the table before decisions become final. I firmly believe that involving discipline-specific experts is essential to fully understand the implications of these closures and to explore viable solutions before a service is lost permanently,” she said.
Note: We’ve reached out to MDI Hospital for comment on the bill and have not heard back before press time. We’ll update if they respond.
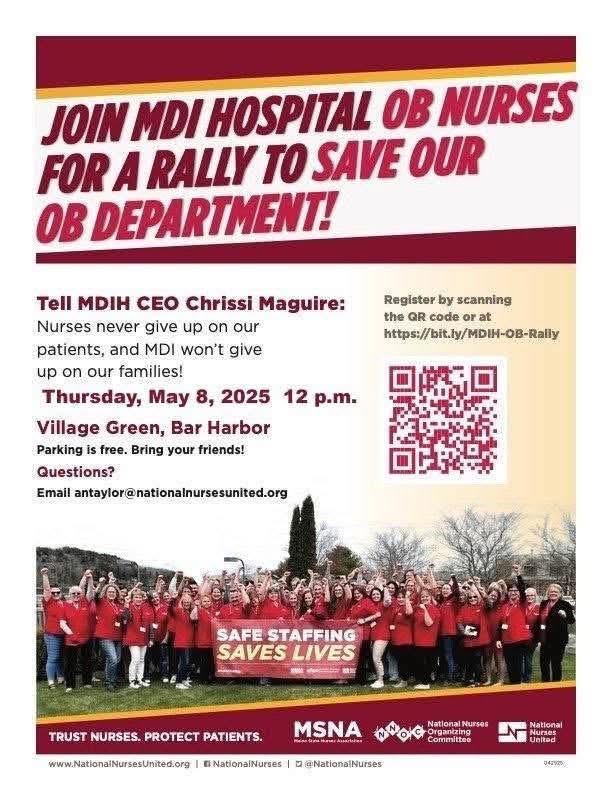
PROTEST SCHEDULED TODAY
LINKS TO LEARN MORE
https://legislature.maine.gov/Audio/#220
https://legislature.maine.gov/billtracker/#Paper/HP1036?legislature=132
https://legislature.maine.gov/billtracker/#Paper/1578?legislature=132
Follow us on Facebook. And as a reminder, you can easily view all our past stories and press releases here.
If you’d like to donate to help support us, you can, but no pressure! Just click here (about how you can give) or here (a direct link), which is the same as the button below.
If you’d like to sponsor the Bar Harbor Story, you can! Learn more here.